Personally, I had never heard about this disorder until I came across a Mental Health YouTuber called Beckie0. She documented the challenges she faced after being diagnosed with Trichotillomania and took a picture of herself for everyday for over 6 years (if my memory is right) she even dedicated a YouTube channel to her and this condition called TrichJournal…which I advise anyone who wants to know more about it in a personal sense to have a look at.

What is Trichotillomania?
Trichotillomania is a condition whereby the individual feels compelled to pull out their hair (this is not limited to pulling but tearing etc). The hair is not limited to their hair on their head but; eyebrows, eyelashes, facial hair, body hair or pubic hair.
This disorder is described by the NHS as an impulse-control disorder, where the individual is physically unable to control or stop them from pulling their hair. The person will feel an intense urge to pull their hair and will not feel relief until they have carried out this behaviour.
As with any mental health condition, Trichotillomania is paired more than likely with negative feelings such as; guilt, depression and anxiety. The person may feel ashamed and embarrassed about their condition and therefore may try to deny or conceal their ‘illness’.
Diagnostic Criteria
A. Recurrent pulling out of one’s hair, resulting in hair loss.
B. Repeated attempts to decrease or stop hair pulling.
C. The hair pulling causes clinically significant distress or impairment to important areas of functioning; social, occupational etc.
D. The hair pulling or hair loss is not attritutable to any other medical condition e.g. dermatological condition.
E. The hair pulling is not better explained as symptoms of another mental disorder e.g. improve perceived defect or flaw in appearance in body dysmorphic disorder.
Diagnostic Features
The essential feature to this condition is the recurrent pulling out of one’s own hair  (Criterion A). Hair pulling can occur from any region of the body in which hair grows; the most common sites according to the DSM are; the scalp, eyebrows and eyelids whilst less common sites
(Criterion A). Hair pulling can occur from any region of the body in which hair grows; the most common sites according to the DSM are; the scalp, eyebrows and eyelids whilst less common sites
are facial and pubic regions. These sites may also vary over time and severity of condition. Hair pulling episodes may occur briefly; scattered throughout the day or during less frequent but more sustained periods that can continue for hours. As such the person may endure hair pulling for months or years. Criterion A requires the hair pulling to result to loss of hair, the individuals with this disorder may pull hair in a vastly distributed pattern therefore hair loss may not be clearly visible. Alternatively the individual may attempt to conceal or camouflage hair loss.
Criterion B acknowledges that individuals with this disorder may make repeated attempts to decrease or stop hair pulling.
Whilst, Criterion C indicates that hair pulling will cause clinically significant distress or impairment in social, occupational and other areas of functioning.
The term distress includes negative affects that may be experienced by a person with this particular condition; feeling a loss of control, embarrassment and shame.
Significant impairment may occur in several areas of functioning and the individual may take part in avoidance behaviours.
Associated Features Supporting Diagnosis
Hair pulling may be accompanied by a range of behaviours or rituals related to or involving hair. A individual may therefore search for a particular kind of hair to pull e.g. pulling hair with a specific texture or colour; they may try to pull out hair in a specific way e.g. the root comes out intact; or may visually examine, tactile or orally manipulate their hair after it’s been pulled e.g. rolling the hair between their fingers, pulling the hair between the teeth, biting the hair or swallowing the hair.
Hair pulling may also be preceded or accompanied by various emotional states; it may be triggered by anxiety or boredom, may be preceded by and increasing sense of tension or may lead to gratification, pleasure or sense of relief. The hair pulling may also involve varying degrees of conscious awareness, some individuals may display more focussed attention to pulling hair whilst for others it may be considered more automatic behaviour (without awareness).
Patterns of hair loss are highly variable; areas of completed alopecia, thinned hair density are common.
Hair pulling according to the DSM-5 does not usually occur in the presence of other people other than family members. However, individuals may have urges to pull hair and therefore may find opportunities to do some surreptitiously. Some individuals may also use replacement and may pull hair from other sources; pets, dolls and other fibrous materials.
The majority of people with Trichotillomania may also have one or more other body-focused repetitive behaviours including; skin picking, nail biting and lip chewing.
Prevalence, Development and Course
The condition is found predominantly in females. It usually develops at an early age from adolescence to early twenties and often can stay with the sufferer throughout their life until they get treatment. Trichotillomania may be present in infants, but the peak age of onset is 9 to 13.
The lifetime prevalence of this disorder is 0.6% of the population (in 2009) leading to 370,752 people possibly affected. However, as with many mental health disorder under-reporting is extremely likely to to the negative emotions associated with the condition.
Causes of Trichotillomania
It’s not known what causes Trichotillomania, but there are several theories. The NHS suggests that this condition may be a type of addiction; the more you pull, the more likely you want to continue the behaviour. It may also be a reflection of other mental health problems; anxiety, depression or stress. In some cases its suggested that this condition may also be a form of self-harm where the person deliberately pulls the hair to seek temporary relief from emotional distress.
Evidence also suggests that the condition can have a genetic link as with OCD.
Treatment
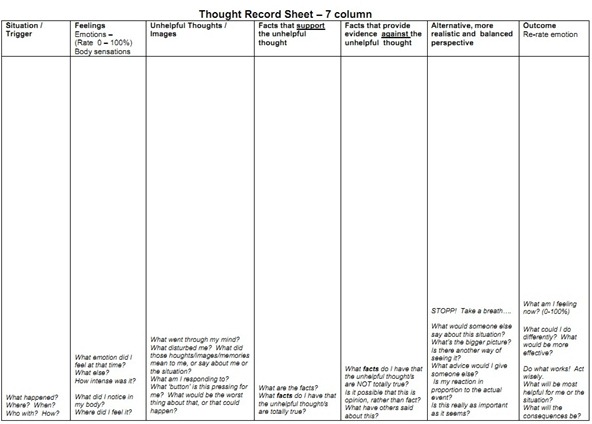
Treatments advised by OCD-UK and evidence based reports link highly to CBT and medication treatment. However, a technique utilised by many cognitive-behavioural therapists is Habit Reversal Training (HRT). This technique was developed in the 1970’s by psychologists Nathan Azrin and Gregory Nunn for treating nervous habits which are done automatically, such as pulling, tics, stammering and skin-picking.
HRT is based on the principle that hair pulling is a conditioned response to specific situations and events, and that the individual with Trichotillomania is unaware of these triggers. Therapy often focuses initially on developing Habit Awareness through the use of journals; why, when and where they pull. HRT challenges the problems of sufferers as a two-fold. Firstly, the individual with Trichotillomania learns how to become more consciously aware of situations and events that trigger hair-pulling episodes. Secondly, the individual learns to utilise alternative behaviours in response to these situations and events. The therapist will encourage individuals suffering from this condition to develop and awareness of the times of day, emotional states and other factors which have lead to hair pulling.
Exposure Therapy has also been utilised in the treatment of Trichotillomania.
Conclusion
Well that’s my best effort at explaining from the DSM what Trichotillomania is, as I have never suffered from this condition I cannot begin to imagine to explain how it makes an individual feel. However, through research and watching Beckie0 on YouTube I have come to understand the condition and the affect it can have on a person. Treatment is available to evaluate thought patterns, behaviours and the urge to pull. Accepting that you are experiencing this condition and reaching out for help is the first step to a journey of learning and potentially changing behaviours.

Further Information;
NHS; http://www.nhs.uk/conditions/trichotillomania/Pages/introduction.aspx










 Body dysmorphic disorder (BDD) is a preoccupation with one or more ‘perceived defects or flaws’ in a persons’ physical appearance that are usually not obvious or appear slightly to others. It is also characterised by repetitive behaviours such as; mirror checking, excessive grooming, skin picking or seeking reassurance from others or mental acts such as; comparing oneself to others. These preoccupations are not better explained by other concerns; body fat, weight or eating disorder.
Body dysmorphic disorder (BDD) is a preoccupation with one or more ‘perceived defects or flaws’ in a persons’ physical appearance that are usually not obvious or appear slightly to others. It is also characterised by repetitive behaviours such as; mirror checking, excessive grooming, skin picking or seeking reassurance from others or mental acts such as; comparing oneself to others. These preoccupations are not better explained by other concerns; body fat, weight or eating disorder. preoccupied with the idea that his or her body build is too small or insufficiently muscular. This specifier is used even if the individual is preoccupied with other body areas, which is often the case.
preoccupied with the idea that his or her body build is too small or insufficiently muscular. This specifier is used even if the individual is preoccupied with other body areas, which is often the case.



 In vivo exposure
In vivo exposure

 If you ask me now am I an emotional person? I would say yes I can be an emotional person; I feel happiness, sadness, joy, empathy, worry but I am not openly emotional anymore. My friend once joked that instead of a heart I had a swinging brick…I have even said this myself. But, this does not mean that I don’t feel the emotions that others would cry at. I feel them, ever perhaps more so than others. When people cry they let the tension, stress, upset go when you don’t have that outlet and don’t have techniques in place you keep that with you, you carry all those feelings around. One of my best friends at university whom I have lived literally next door too for 3 years minus the Christmas and festive breaks I would say has only seen me cry a handful of times, especially where alcohol hasn’t been involved! Does it mean that I am not open with my emotion? No. I just display my emotions differently I have already touched on hiding behind a smile and using humour and that’s just what I do. I can talk about what some would view as traumatic events, stressful situations til the cows come home yet I would not cry I may get a ‘frog in my throat’ and choke up a little but I just don’t cry. Well not infront of ‘large’ audiences anyways!
If you ask me now am I an emotional person? I would say yes I can be an emotional person; I feel happiness, sadness, joy, empathy, worry but I am not openly emotional anymore. My friend once joked that instead of a heart I had a swinging brick…I have even said this myself. But, this does not mean that I don’t feel the emotions that others would cry at. I feel them, ever perhaps more so than others. When people cry they let the tension, stress, upset go when you don’t have that outlet and don’t have techniques in place you keep that with you, you carry all those feelings around. One of my best friends at university whom I have lived literally next door too for 3 years minus the Christmas and festive breaks I would say has only seen me cry a handful of times, especially where alcohol hasn’t been involved! Does it mean that I am not open with my emotion? No. I just display my emotions differently I have already touched on hiding behind a smile and using humour and that’s just what I do. I can talk about what some would view as traumatic events, stressful situations til the cows come home yet I would not cry I may get a ‘frog in my throat’ and choke up a little but I just don’t cry. Well not infront of ‘large’ audiences anyways!


 incident or trauma. Particularly in childhood, if for example a child is bitten by a dog then they may develop a specific phobia of dogs. If a person is suffering from ‘agoraphobia’ it may be related to a specific trauma such as; a car accident, or sexual attack these may cause a person to feel unsafe in open situations or when they aren’t at home.
incident or trauma. Particularly in childhood, if for example a child is bitten by a dog then they may develop a specific phobia of dogs. If a person is suffering from ‘agoraphobia’ it may be related to a specific trauma such as; a car accident, or sexual attack these may cause a person to feel unsafe in open situations or when they aren’t at home.
 there is evidence to suggest that some people are born with vulnerabilities to have a tendency to be more anxious than others. This vulnerability may make it easier for phobias to develop.
there is evidence to suggest that some people are born with vulnerabilities to have a tendency to be more anxious than others. This vulnerability may make it easier for phobias to develop.







 Relaxation techniques that can be utilised in depressive/low mood and anxiety are;
Relaxation techniques that can be utilised in depressive/low mood and anxiety are;

 expression and communication through any form of art; it allows the person to explore what they are creating and discuss in a safe environment these creations; it facilitates self-expression. Art therapy allows the person to talk about themselves through the medium of art. The art helps to open communication channels and self-awareness. Expression of emotions can also
expression and communication through any form of art; it allows the person to explore what they are creating and discuss in a safe environment these creations; it facilitates self-expression. Art therapy allows the person to talk about themselves through the medium of art. The art helps to open communication channels and self-awareness. Expression of emotions can also 




 This form of cognitive thinking error quite literally means the person filters out all the positive thinking and magnifies negative details of the particular situation. For example, a person may obsess over a negative detail of a situation and dwelling on this for a significant period of time may become their version of distorted reality.
This form of cognitive thinking error quite literally means the person filters out all the positive thinking and magnifies negative details of the particular situation. For example, a person may obsess over a negative detail of a situation and dwelling on this for a significant period of time may become their version of distorted reality. We have to be perfect or we are a failure. The person places others and situations in categories of ‘either’/’or’. For example, if a person doesn’t achieve the best grade possible an A but receives an B they are a failure despite recieving a very good grade. Personally, I am a perfectionist and I am well aware of this. I commonly used to utilse this thinking error especially when discussing academic or voluntary work. If some things worked out yet if one particular area the thing that worked well wouldn’t matter.
We have to be perfect or we are a failure. The person places others and situations in categories of ‘either’/’or’. For example, if a person doesn’t achieve the best grade possible an A but receives an B they are a failure despite recieving a very good grade. Personally, I am a perfectionist and I am well aware of this. I commonly used to utilse this thinking error especially when discussing academic or voluntary work. If some things worked out yet if one particular area the thing that worked well wouldn’t matter. n this error a person draws a general conclusion based on a single event or single piece of evidence. If something bad only happens once, the person may expect it to happen again. A person may see this form of thinking as a never-ending defeat in their eyes.
n this error a person draws a general conclusion based on a single event or single piece of evidence. If something bad only happens once, the person may expect it to happen again. A person may see this form of thinking as a never-ending defeat in their eyes. eling and why they act in particular ways. In particular we are able to know how a person thinks or feels
eling and why they act in particular ways. In particular we are able to know how a person thinks or feels This thinking pattern convinces the person that disaster will strike in any particular situation. We hear about a situation and we use ‘what if’ statements always focusing on the negative in the situation. For example, a person might exaggerate the importance of insignificant events (such as their mistake) and minimise the magnitude of significant events (what the person is good at).
This thinking pattern convinces the person that disaster will strike in any particular situation. We hear about a situation and we use ‘what if’ statements always focusing on the negative in the situation. For example, a person might exaggerate the importance of insignificant events (such as their mistake) and minimise the magnitude of significant events (what the person is good at). at others do or say is a direct reaction to the person. For example, people laughing at the back of the bus
at others do or say is a direct reaction to the person. For example, people laughing at the back of the bus do this you compare yourself to others who you feel have an advantage to you or are better at something than you. These unfair comparisons leaves the person feeling inadequate and can reinforce negative thinking about themselves and may strengthen self-hatred.
do this you compare yourself to others who you feel have an advantage to you or are better at something than you. These unfair comparisons leaves the person feeling inadequate and can reinforce negative thinking about themselves and may strengthen self-hatred.