This disorder as with many mental health conditions has been within the public eye through the use of television programmes based on Hoarding such as; Obsessive Compulsive Hoarder, The Hoarder Next Door and Britain’s Biggest Hoarders. These are often presented as extreme cases whereby other services have had to become involved to help the person discard personal possessions.
So, what is Hoarding?
Hoarding disorder is characterised by persistent difficulty discarding or parting with possessions, regardless of their value as a result of a strong perceived need to save the items and the distress associated
with parting from them. This disorder however differs from ‘normal collecting’ as, the symptoms of this disorder result in the accumulation of a large number of possessions that take over, clutter active living areas to the extent that their intended use is substantially compromised. This disorder consists of excessive collecting, buying or stealing items that are not actually recquired for which there is no available space and stored in a chaotic manner.
Diagnostic Criteria
A. Persistent difficulty discarding or parting with possessions, regardless of their actual value.
B. This difficult is due to the perceived need to save the items and to distress associated with discarding them.
C. This difficulty discarding possessions results in the accumulation of possessions that congest and clutter active living areas and substantially compromises their intended use. If living areas are uncluttered, it is only because of the interventions of third parties e.g. family members, authorities or cleaners.
D. The hoarding causes clinically significant distress or impairment in social, occupational,or other important areas of functioning (including maintaining a safe environment for self and others).
E. The hoarding is not attributable to another medical condition (e.g., brain injury, cerebrovascular disease, Prader-Willi syndrome).
F. The hoarding is not better explained by the symptoms of another mental disorder (e.g.,obsessions in obsessive-compulsive disorder, decreased energy in major depressive disorder, delusions in schizophrenia or another psychotic disorder, cognitive deficits in
major neurocognitive disorder, restricted interests in autism spectrum disorder).
Specifiers
With excessive acquisition; to put it bluntly this specifier is linked with the nature of acquisition’…e.g. the extreme severity of the situation- are they buying these possessions? Sought out for free or stolen?
According to the DSM-5, approx. 80-90% of individuals display excessive acquisition. The most frequent form of acquisition is excessive buying, followed by acquisition of free items e.g. leaflets. Stealing is less common. Some people deny excessive acquisition when first assessed, yet it may appear later in their course of treatment. Individuals typically experience distress if they are unable or prevented from acquiring items.
With good or fair insight; the person recognises that their beliefs are problematic.
With poor insight; the person recognises that their beliefs and behaviours are not problematic despite evidence on the contrary.
With absent insight/ delusional beliefs; The person is utterly convinced that their beliefs and behaviours are not problematic despite contrary evidence.
Diagnostic Criteria
The essential feature of hoarding is the persistent difficulties discarding parting with possessions, regardless of actual value (Criterion A).
The term persistent indicates a long-standing difficulty rather than more transient life circumstances that may lead to excessive clutter e.g. inheriting a property.
The difficulty in discarding possessions refers to any form of discarding e.g. throwing away, selling, giving away or recycling. The main reasons for these issues are due to the perception that the possessions can be utilised, may have aesthetic value or sentimental attachment. Some individuals feel responsible for the fate of their possessions and often go to great lengths to avoid waste. Fear of losing important information is also common. Commonly saved items are; newspapers, magazines, old clothing, bags, books, mail and paperwork but virtually any item can be saved or hoarded. It must also be noted that hoarded items do not have to have little value but can also be more valuable and these items can be seemingly mixed with the clutter and chaotic hoarded possessions.
People with hoarding disorder purposefully save possessions and experience distress when facing the prospect of discarding them (Criterion B). This criteria emphasises that saving these possessions are intentional, which discriminated hoarding disorder from other forms of mental illness that are characterised by the passive accumulation of items or the absence of distress with the items are removed.
Individuals accumulate large numbers of items that fill up and clutter active living areas to the extent that their intended use is no longer possible (Criterion C). For example, the person may not be able to prepare food in their kitchen or are forced to sleep on their sofa. If the space can be used, it is only with great difficulty.
Clutter is defined as a large group of usually unrelated or marginally related objects piled together in a disorganised fashion in spaces designed for other purposes e.g. tabletops, floors, hallway.
Criterion C emphasises the ‘active living areas’ of the hom
e, rather than more peripheral areas such as; garages, attics or basements, that are usually cluttered in homes where people do not suffer from Hoarding disorder. However, people with hoarding disorder often have possessions that spill beyond the active living areas and occupy and impair the use of living spaces and other spaces such as; vehicles, yards, gardens and storage spaces. In some cases however, living areas may be uncluttered due to the intervention of third parties such as family members this may then force the person to undertake renting storage units or using other spaces to hold their possessions.
Hoarding disorder is distinctively different from normal collecting behaviour as collecting is usually systematic and organised. The actual amount of possessions may be similar however the storage of these possessions is obviously different as normative collecting does not produce the clutter, distress or impairment of typical hoarding disorder.
Criterion D outlines that symptoms must cause clinically significant distress or impairment in normal functioning. In some cases where a person has poor insight the person may not report distress and the impairment may be only apparent to people around them. However, any attempts to discard or clear the possessions by other parties results in high levels of stress.
Prevalence, Development and Course of Hoarding Disorder
Figures from Help for Hoarders UK suggest that approximately 2-5% of the UK population, potentially over 1.2 million people suffer from Hoarding disorder where clinical, psychological help may be required.
According to the DSM-5 Hoarding Disorder affects both males and females however, epidemiological studies suggest that there is a significantly greater prevalence in males compared to clinical samples which predominantly feature females.
Hoarding symptoms appear to begin early in life and spans well into late stages of life. These symptoms are reported to emerge around ages 11-15 years old, they start to interfere with daily functioning in the mid 20’s and cause clinically significant impairment by the mid-30’s. Once symptoms are presented of Hoarding the course of hoarding is often chronic as these symptoms tend to increasingly become more severe throughout their life span.
Risk and Prognostic Factors
Tempremental; Indecisiveness according to the DSM is a prominent featutre of an individual with hoarding. As they are unable to come to a clear decision about whether a possession may be required in the future and therefore keep it to be on the safe side.
Environmental; Individuals with hoarding disorder often retrospectively report stressful and traumatic life events preceding to the onset of the disorder or the traumatic event may exacerbate the development of the disorder.
Genetic and Physiological; Hoarding disorder is believed to be familial with about 50% of people who hoard report having a relative whom also hoards. Twin studies suggest that 50% of variability in hoarding behaviour is due to genetic factors.
Interaction; The DSM states that their is evidence to suggest a genetic link to hoarding disorder. However, this may also be due to the person’s environment; sharing environments with a person who hoards may impart beliefs and understanding within their own children’s mind which may increase the likelihood of them picking up on hoarding behaviours and developing the disorder themselves.
GENETICS + ENVIRONMENT = POTENTIAL DISORDER
Treatment
The NHS website outlines the treatment for individuals suffering from Hoarding Disorder. These treatments include; CBT, SSRI medication treatment. I would also suggest Exposure therapy may also be helpful for the person to gain insight and gradually understand that these possessions do not necessarily need to be kept and understand their own thought patterns behind the behaviour.
Conclusion
Hoarding although chronic in course and can affect a persons life increasingly treatments have been seen to be effective in retraining a persons thought patterns and behaviours to acknowledge that the do not need to keep hold of possessions that are not required. These treatments may help the person to gain insight into their illness and try to understand why they hold beliefs about discarding possessions. Successful support and assistance however is the most important step. Treating someone with CBT away from the hoarding environment may prove to be ineffective, truthfully individuals need to be treated at home where their disorder stems from and disrupts to truly make a difference.
Personally, I am quite a sentimental person so I do have memory boxes on my bookshelf and a jar full of corks from special events which I am going to reuse and make into some art…you may see it eventually. I wouldn’t say I’m a hoarder in the slightest but I do attach sentimental values to items I suppose if I was a good at writing journals or scrapbooks then the memory boxes may be different but lets face it this blog I suppose could be considered hoarding of information and memories lets just remember the look back over 2015 posts. As with any mental condition it comes down to the person’s ability I believe to cope effectively if their disorder is clinically distressing and impedes on their life then clearly some intervention is required but I wouldn’t say that keeping hold of things which are sentimentally significant is a bad thing because well I do it. So please don’t think that I think keeping things that are sentimentally valuable or collecting things that you may feel is valuable or necessary is a bad thing, it is just when these need to keep and not discard anything impinges on your life that these beliefs and behaviours need to be addressed.

Further Information;
NHS;http://www.nhs.uk/conditions/hoarding/Pages/Introduction.aspx
OCD UK; http://www.ocduk.org/hoarding










 some cultures this may be known as an experience of possession). The disruption in identity involves marked discontinuity in sense of self and sense of agency accompanied by related alterations in affect, behaviour, consciousness, memory, perception, cognition and/or sensory-motor functioning. This signs and symptoms may be observed by others or reported by the individual.
some cultures this may be known as an experience of possession). The disruption in identity involves marked discontinuity in sense of self and sense of agency accompanied by related alterations in affect, behaviour, consciousness, memory, perception, cognition and/or sensory-motor functioning. This signs and symptoms may be observed by others or reported by the individual.
 individual. For instance;
individual. For instance; memory for long periods of time or of memories involving the traumatic event.
memory for long periods of time or of memories involving the traumatic event. These symptoms are related to the individuals arousal of certain physiological aspects. The individual may suffer from sleep disturbance (difficulty falling or staying asleep), irritability and anger outbursts (with little or no provocation) typically verbal of physical aggression towards people or objects, hypervigilance, problems with concentration and exaggerated startle response (being on edge).
These symptoms are related to the individuals arousal of certain physiological aspects. The individual may suffer from sleep disturbance (difficulty falling or staying asleep), irritability and anger outbursts (with little or no provocation) typically verbal of physical aggression towards people or objects, hypervigilance, problems with concentration and exaggerated startle response (being on edge).


 your name you still need valid in some cases paid experience and that is what I plan on doing in the intervening year. As my Dad has said in many occasions life is a marathon not a sprint at the end of the day I am 21 years old, have a mature head on my shoulders (if I do say so myself) and I have another 50 years of my working life ahead I’m not expecting to walk into my dream job straight away and I’m definitely not afraid of working hard to get there.
your name you still need valid in some cases paid experience and that is what I plan on doing in the intervening year. As my Dad has said in many occasions life is a marathon not a sprint at the end of the day I am 21 years old, have a mature head on my shoulders (if I do say so myself) and I have another 50 years of my working life ahead I’m not expecting to walk into my dream job straight away and I’m definitely not afraid of working hard to get there.


 On a mental health note; I have recently reduced my anti-depressants; I’m not sure if anyone actually knows about this. So I decided that it was about time to reduce my anti-depressant Sertraline. Now, let me make this clear I have not had any medical assistance. After quite a few years of being stable on 100mg of Sertraline- 3 years in March (oh how time flies when you are having fun) I didn’t feel ‘depressed’ but I knew I wasn’t feeling right. I have always been able to know how I’m feeling I think its my awareness related to my diabetes.
On a mental health note; I have recently reduced my anti-depressants; I’m not sure if anyone actually knows about this. So I decided that it was about time to reduce my anti-depressant Sertraline. Now, let me make this clear I have not had any medical assistance. After quite a few years of being stable on 100mg of Sertraline- 3 years in March (oh how time flies when you are having fun) I didn’t feel ‘depressed’ but I knew I wasn’t feeling right. I have always been able to know how I’m feeling I think its my awareness related to my diabetes. 







 (Criterion A). Hair pulling can occur from any region of the body in which hair grows; the most common sites according to the DSM are; the scalp, eyebrows and eyelids whilst less common sites
(Criterion A). Hair pulling can occur from any region of the body in which hair grows; the most common sites according to the DSM are; the scalp, eyebrows and eyelids whilst less common sites







 Body dysmorphic disorder (BDD) is a preoccupation with one or more ‘perceived defects or flaws’ in a persons’ physical appearance that are usually not obvious or appear slightly to others. It is also characterised by repetitive behaviours such as; mirror checking, excessive grooming, skin picking or seeking reassurance from others or mental acts such as; comparing oneself to others. These preoccupations are not better explained by other concerns; body fat, weight or eating disorder.
Body dysmorphic disorder (BDD) is a preoccupation with one or more ‘perceived defects or flaws’ in a persons’ physical appearance that are usually not obvious or appear slightly to others. It is also characterised by repetitive behaviours such as; mirror checking, excessive grooming, skin picking or seeking reassurance from others or mental acts such as; comparing oneself to others. These preoccupations are not better explained by other concerns; body fat, weight or eating disorder. preoccupied with the idea that his or her body build is too small or insufficiently muscular. This specifier is used even if the individual is preoccupied with other body areas, which is often the case.
preoccupied with the idea that his or her body build is too small or insufficiently muscular. This specifier is used even if the individual is preoccupied with other body areas, which is often the case.



 This condition is incredibly debilitating and disabling as it affects many areas of a persons life. The World Health Organisation (WHO) has ranked OCD as being in the top 10 of the most disabling illnesses of any kind in terms of its lost earnings and diminished quality of life.
This condition is incredibly debilitating and disabling as it affects many areas of a persons life. The World Health Organisation (WHO) has ranked OCD as being in the top 10 of the most disabling illnesses of any kind in terms of its lost earnings and diminished quality of life.

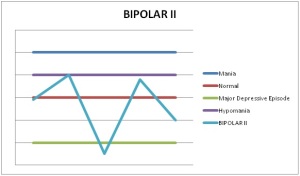
 Lithium is probably one of the most well-known treatments for people with Bipolar disorder. This form of medication can be very effective treatment for mania, but is less effective in treating symptoms of Depression (Smith,2012). It helps to reduce the severity and frequency of mania, and is often the long-term method of treating Bipolar disorder (Geddes et al., 2004).Evidence suggests that Lithium is most effective for;
Lithium is probably one of the most well-known treatments for people with Bipolar disorder. This form of medication can be very effective treatment for mania, but is less effective in treating symptoms of Depression (Smith,2012). It helps to reduce the severity and frequency of mania, and is often the long-term method of treating Bipolar disorder (Geddes et al., 2004).Evidence suggests that Lithium is most effective for;
 Some people suffering from Bipolar disorder may be prescribed anti-depressants. A commonly prescribed anti-depressant is SSRI’s (selective serotonin re-uptake inhibitors- see ‘The strive for the right medication’ for an explanation of SSRI’s).
Some people suffering from Bipolar disorder may be prescribed anti-depressants. A commonly prescribed anti-depressant is SSRI’s (selective serotonin re-uptake inhibitors- see ‘The strive for the right medication’ for an explanation of SSRI’s).